Lack of evidence is key barrier to using portable devices to detect poor quality medicines
A series of papers which reviewed portable devices to detect poor quality medicines has concluded major gaps in scientific evidence remain a key barrier for regulators to implement surveillance systems using such devices.
The five papers have been published in PLOS Neglected Tropical Diseases and PloS Medicine today. They are:
1. Multiphase evaluation of portable medicines quality screening device
2. Laboratory evaluation of twelve portable devices for medicine quality screening
3. A comparative field evaluation of six medicine quality screening devices in Laos.
Poor quality medical products jeopardise national, regional and global attempts to improve access to effective health care because they lead to avoidable morbidity and mortality, waste human and financial resources, and contribute to drug resistance. The World Health Organization estimates that globally 1 in 10 medical products is substandard and falsified (SF*), but the reality is that their detailed epidemiology remains very unclear because of the difficulties of detecting them in supply chains and communities.
Medicines Regulatory Authorities (MRAs) in many low-and middle-income countries are under-resourced. New innovative portable tools could help improve MRA efficiency in post-market surveillance of medicines, to better detect and remove SF medicines before they reach patients. Although they hold promise for empowering medicine inspectors in screening medicine quality in supply systems, regulators lack independent information on their performance, limitations and cost-effectiveness. This study aimed to help fill this gap in our understanding.
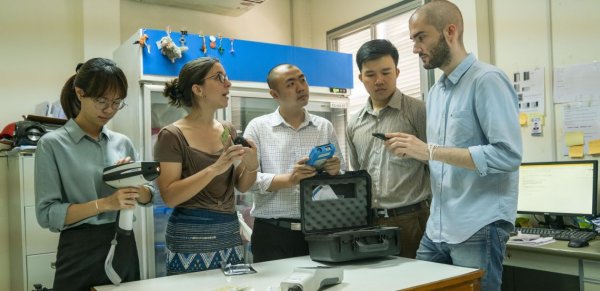
The Medicine Quality Research Group (LOMWRU, Lao PDR) of IDDO and the Mahidol Oxford Tropical Medicine Research Unit (MORU) worked in collaboration with the Government of the Lao PDR, the Georgia Institute of Technology (USA) and MORU in Thailand to conduct an independent evaluation and comparison of portable devices to provide evidence to facilitate MRAs decisions about whether these new technologies are appropriate for screening of medicines in their countries and they should be deployed. The study was part of the Results for Malaria Elimination and Communicable Diseases Control (RECAP) under the Regional Malaria and Communicable Disease Trust Fund (RMTF) at the Asian Development Bank. This work has been described in this series of five papers.
Twelve portable devices were chosen following a review of the available scientific evidence. These ranged from small single-use rapid diagnostic test kits, through to small spectrometers that can be connected to mobile phones, hand-held spectrometers, and larger devices such as the Minilab, a laboratory in suitcases. Each device was evaluated in the laboratory, the field and for cost-effectiveness. Download more information about the evaluation process
The study’s key findings increase our knowledge of the use of these devices but show that it is currently unlikely that any one device would be able to effectively monitor the quality of all medicines. The researchers concluded that major gaps in the scientific evidence remain and are key barriers for regulators wishing to implement devices in their surveillance systems. However, these devices, when their advantages and limitation are better defined for diverse medicines hold great promise for empowering medicine inspectors globally.
Read the papers
- Multiphase evaluation of portable medicines quality screening devices.
- Laboratory evaluation of twelve portable devices for medicine quality screening
- A comparative field evaluation of six medicine quality screening devices in Laos.
- Implementation of field detection devices for antimalarial quality screening in Lao PDR—A cost-effectiveness analysis.
- Evaluation of portable devices for medicine quality screening: Lessons learnt, recommendations for implementation, and future priorities
* About SF medical products
Substandard medical products result from errors and negligence during manufacture, transportation, or storage. In contrast, falsified products result from criminal fraud. Although they have been traded for many centuries, in the last few decades the problem seems to have grown, partly because of the increased complexity of the global pharmaceutical economy and internet sales.
