Analysing malaria treatments in Africa: a comparison of the two front-line treatments
A statistical analysis of data hosted within the WWARN repository from 4,214 participants across multiple study sites in Africa has been published in BMC Medicine. Results indicate that the local prevalence of resistance-associated markers should be considered when choosing a first-line drug to ensure optimal duration of protection.
In Africa, most cases of P. falciparum malaria are treated with the artemisinin combination therapies, primarily artemether-lumefantrine (AL) and artesunate-amodiaquine (AS-AQ). Despite emerging resistance to components of these treatments at different levels around the world, both AS-AQ and AL remain highly effective in most malaria-endemic areas of Africa. The pharmacokinetic properties of these drugs are fairly well characterised but what is less clear, is their length of effectiveness post-treatment. The duration of protection can contribute to reducing morbidity in highly-exposed individuals and reduce overall transmission in the community.
There has been some evidence that the duration of protection after AS-AQ and AL treatment is affected by genetic mutations in malaria parasites, which may reduce the sensitivity of the drugs. These genetic markers of resistance are thought to reduce sensitivity to AS-AQ, but increase sensitivity to AL.
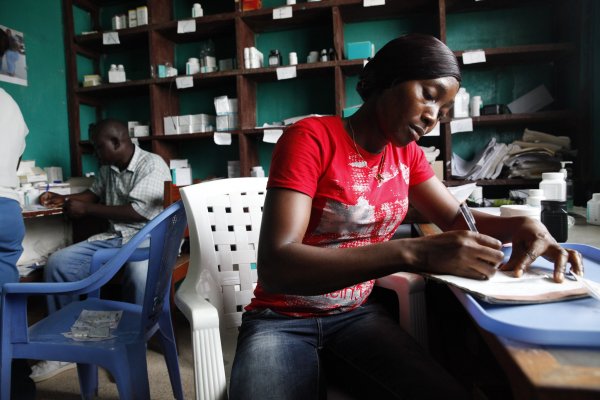
WWARN's AS-AQ and AL post-treatment prophylaxis Study Group conducted a statistical analysis of pooled clinical trial data from the WWARN Malaria Data Inventory. Clinical trials were included that monitored reinfection rates and the analysis took account of local transmission intensity to estimate the duration of protection of AS-AQ and AL.
Two different statistical approaches were used to estimate the duration of post-treatment effectiveness and to understand factors that modify this (hidden Semi-Markov models and accelerated time failure models). Authors then used a mathematical model to simulate the epidemiological consequences of using AS-AQ versus AL as first-line treatments.
It was found that the duration of protection between the two drugs varied considerably across trial sites and that there was no one size fits all. In some cases, AS-AQ provided an estimated 19 days of protection, more than twice that of AL, whereas in other sites the reverse was true. This appears to be due to the local prevalence of mutations in the parasites at the time the trial was conducted. AS-AQ provided better protection in areas where parasites did not have mutations and AL performed better where mutations in the parasites were more common, in line with previous findings.
Dr Lucy Okell, from Imperial College London, and lead author on the study says: "The simulations found that these differences in the duration of protection could alter the incidence of malaria by up to 14% in children under five in areas with high, seasonal transmission. These results have important potential consequences as young children are one of the most vulnerable groups affected by malaria. 61% of deaths from malaria in 2017 were in children under five."
The authors recommend that when choosing a first-line treatment, the local prevalence of resistance-associated markers should be considered to ensure optimal reduction of malaria. They also emphasize the importance of continuing to monitor for other resistance markers in future.
Read the paper: The duration of chemoprophylaxis against malaria after treatment with artesunate-amodiaquine and artemether-lumefantrine and the effects of pfmdr1 86Y and pfcrt 76T: a meta-analysis of individual patient data. BMC Medicine. 25 February 2020
This work was done as part of WWARN's AS-AQ and AL post-treatment prophylaxis Study Group
